Care Island
A self-guided tool for navigating the first days after a cancer diagnosis.
I led a safety-first reframe, focusing on emotional stabilization before resource orchestration, so that action feels possible, not paralyzing.
AT A GLANCE
CLIENT: UPMC Macgee Hospital
TIMELINE: 12 WEEKS
TEAM: Three person interdisciplinary team: engineering, service design, research
MY ROLE:
I led UX research and originated concepts, grounding them in shadowing sessions with oncology teams, interviews with patients and caregivers, and journey mapping transitions of care.
OUTCOME BENEFITS:
Prototype adoption from UPMC Magee. Positive reception from patient cohort (n=8); participants reported greater emotional clarity, a sense of grounding, and willingness to reuse the tool.
OVERVIEW
PATIENT QUOTES
A diagnosis. A portal. No one to talk to.
Gynocology oncology patients at UPMC Macgee were receiving their cancer diagnosis through a portal, with no guidance, preparation, or conversation.
What is Care Island?
Care Island is a self-guided digital tool designed to support patients in the emotional “in-between”: the days right after diagnosis, before care begins.
This made me feel emotional, and it felt super real. The game felt patient with me, like I was slowly building support instead of having it all thrown at me.— Patient Participant
I truly wish I had this when I was going through that time in my life. (This) almost made me cry.— Patient Participant
The music and pacing made it feel less like a little game and more like a tool I could actually rely on.— Patient Participant
This is one of the transitions (of oncology) that lacks the most support...maybe on purpose. Your methods felt unobtrusive and uplifting.— Clinician Reviewer

WHERE IT BEGAN
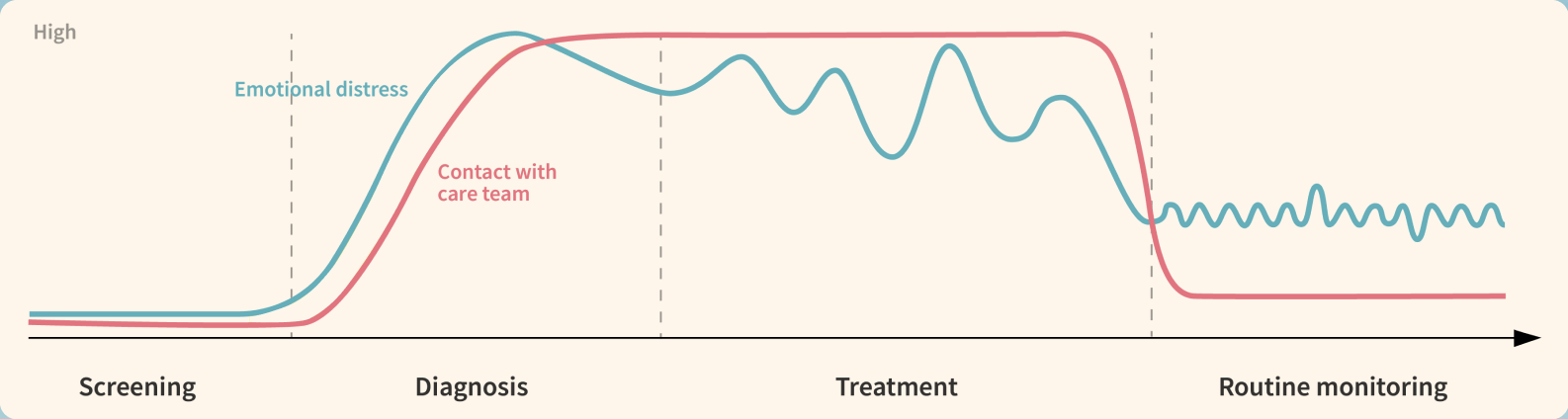
Research goal: How might we enable patients and caregivers to ask the right questions at the right time during all transitions of care?
Our sensemaking map of oncological journey + key transitions of care
RESEARCH APPROACH
From 150+ field observations through shadowing, we found three key experience gaps we had to address:
To capture experiences across perspectives, I used a multi-method approach:
8 patient shadowing sessions during oncology visits and waiting rooms
9 caregiver and patient interviews about emotional and logistical challenges
5 clinician interviews to understand care transitions
1 co-design workshop with 6 patients to test prototypes and explore interventions
AS SEEN IN THE ROOM
Patients were overwhelmed by disorganized info and retained little post-visit, leading to anxious, unproductive Googling.
Narrow to a single, doable action patients can revisit and control.
→ Leads to: 72-hour pathway
Small talk in waiting rooms or having an idea of a plan became anchors—tiny things that helped people feel human again.
Brief, calming prompts to re-center before surfacing tasks or info.
→ Leads to: Reflective “island” moments
Patients were expected to make huge decisions quickly, but no one was helping them bridge that gap.
Make contacting care and updating loved ones easy, without reply pressure.
→ Leads to: Call-ready script + optional broadcast

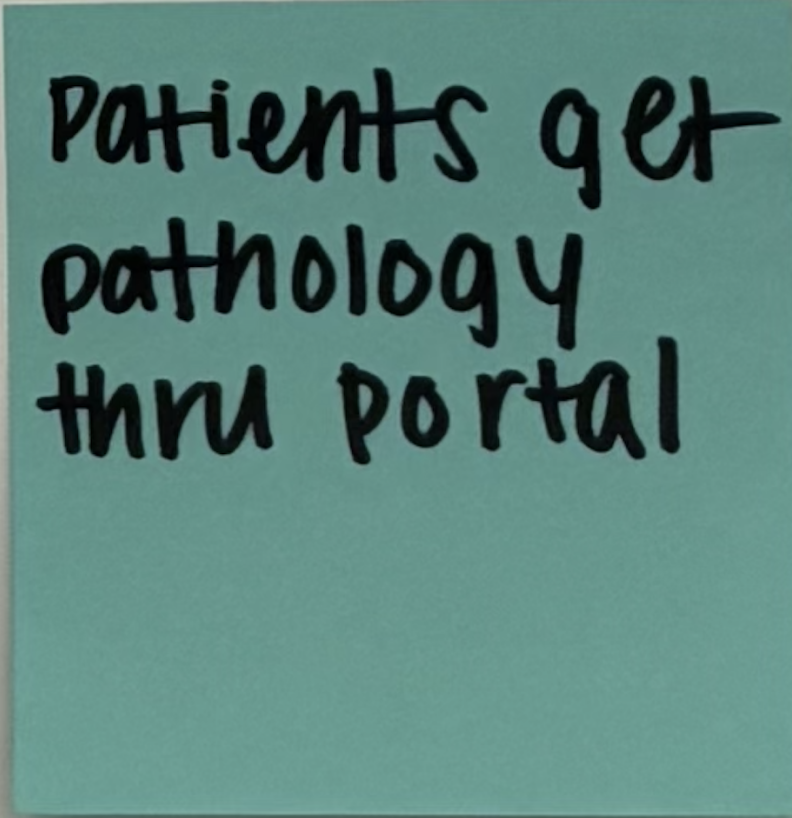
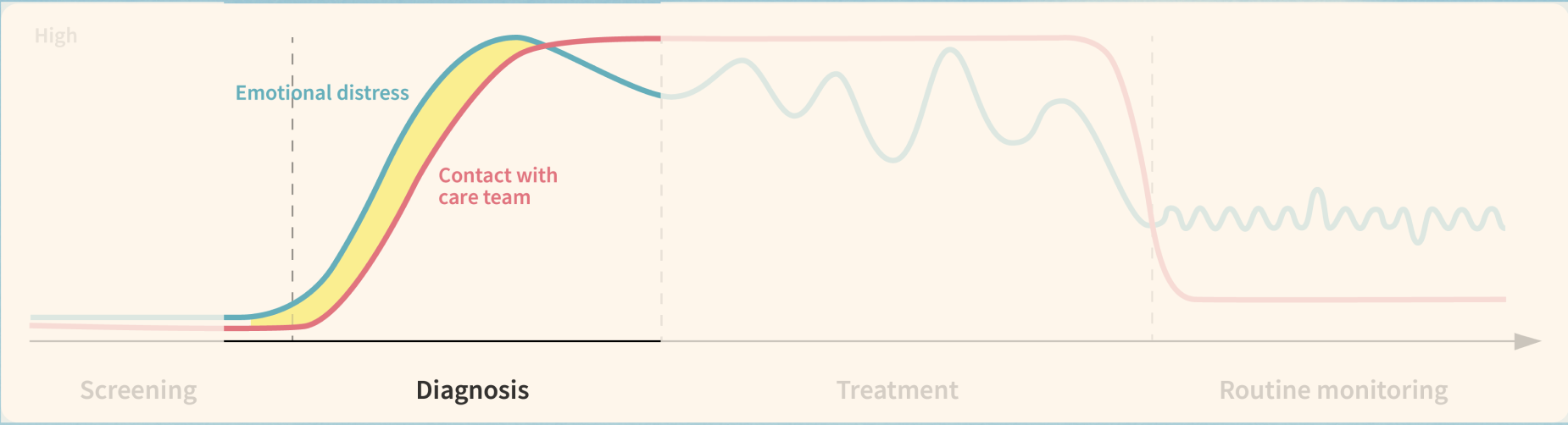
This field note reframed our whole approach.
“Patients get pathology through the portal.” This observation made us realize that patients weren’t just overwhelmed, but they were alone at the moment of receiving their diagnosis.
Our solutioning pivoted from providing information during all the transitions of care, to emotional readiness at the just the specific diagnosis moment, where confusion, disorientation, and stress spikes.
I worked with the clinicians and stakeholders to reframed our inquiry toward new research questions:
What happens in the immediate moment of receiving a diagnosis digitally?
How might design interventions provide grounding and emotional readiness at that specific time?
FROM FIELDWORK TO FRAMING
I facilitated a structured co-design workshop to understand how patients engaged with prototypes and the stories that shaped their responses.
-
Caregivers need tools too, to help process without intrusion.
-
Participants wanted to be asked how they feel about their diagnosis, rather than being bombarded with choices.
-
Patients didn’t want onboarding instructions that added to their cognitive load.
“Your brain just can’t handle that much news and change, all at once.”
- Caregiver
DIGGING DEEPER
DIARY STUDY STORIES
A patient’s story became my compass.
After getting the news, gyn-onc patient Rachel retreated at a rural Airbnb, dictating what information reached her and when, and how her loved ones behaved to ease her anxiety. She called it her “island.”
Not every patient has the same resources or support system as Rachel, which led us to our north-star question:
When the ground shifts beneath you, what does it mean to build a place that’s just yours?
INTRODUCING: CARE ISLAND
Our solution: A gentle, self-guided game to ground newly diagnosed cancer patients in their first uncertain days.
Why a game?
After diagnosis, patients face extreme emotional overload. Trauma informed research papers dove into show that slow, reflective gameplay can support processing, agency, and self-connection. We chose four specific features to pilot based on interviews and secondary research determining which exercises would be most grounding and necessary during this time, including defining roles for loved ones, breathing intentionally, and finding comfort in daily activities.
KEY FEATURES AND METAPHORS
Each token stands on island, an activity that user completes and represents the support they have control over.
Support system campfire
Who can be there for you? And how?
Comfort menu
What are some things you can do?
Through simple, reflective activities, patients add elements to their island, each one a reminder of the support around them and the control they still hold.
Grounded in research, Care Island helps patients reclaim:
Support: visible anchors of care and connection
Control: a sense of agency at a time that often feels powerless
In the end, the island becomes both a tool and a symbol: a personal refuge patients can return to when the ground feels unsteady.
Grounding Pond
What information do you have control over?
Companion symbol
Who quietly guides you through uncertainty?

REFLECTING
IF I HAD MORE TIME…
This was one of the most raw, emotional, and meaningful projects I’ve worked on. It changed how I practice, pushing me to design from sincerity while being honest about healthcare constraints. I learned specifically:
Why restraint and simplicity are critical when designing for overwhelmed users.
The power of co-creation and involving patients at every step.
How metaphors and physicality can make experiences feel more human and joyful!
Fieldwork also showed that “faster access” at diagnosis isn’t realistic or safe, which led me to a constraints-aware, psychology-informed pivot, so patients can act without spiraling. Our literature review on cognitive load and trauma-aware communication reinforced sequencing emotional grounding before information.
Now: Care Island is in active use with our UPMC Magee cohort and moving into a structured pilot.
Next:
Tighten signals: quick icon emotion read + copy/tone pass so visuals/words calm, not spike.
Verify effect: add a tiny pre/post “at-ease” check around each activity.
Track impact: instrument time-to-first-action (≤72h) and % arriving with prepared questions.